
- Why us?
- Company
-
Services
Our Service
-
Technology
-
News & Resources
Clinic Resources
I have covered this topic briefly on a number of occasions, but it so poorly understood and confusing, that it deserves its very own “Fun with ECGs”.
The vagus nerve slows sinus rhythm. It innervates the sinus node via ganglia adjacent to the superior vena cava and epicardial right atrium with innervation predominantly from the right vagus nerve. Similar innervation lies adjacent to the AV node, predominantly from the left vagus. There is significant cross-innervation.
Respiratory sinus arrhythmia is a benign normal variation in heart rate, that occurs during each respiratory cycle; heart rate increases with inspiration and slows with expiration. With inspiration, the diaphragm is lowered, the lungs inflate and blood pools in the chest. The result is a reduced volume of blood returning to the atrium resulting in an increase in heart rate. During expiration, the opposite happens. Sinus arrhythmia occurs at all ages but is most prominent in the young and elderly.

Sinus arrhythmia is best seen during Holter monitoring, because with a 12-lead ECG, the patient is often told to hold their breath. There may also be an exaggerated response if the patient takes a deep inspiration, immediately before the ECG.
At night during sleep, the vagal response may be exaggerated particularly in response to changes in respiration. This increased tone, referred to as vagal hypertonia may result in an impressive array of ECG appearances. The following ECGs are mainly Holter monitor recordings at night in young patients or athletes.
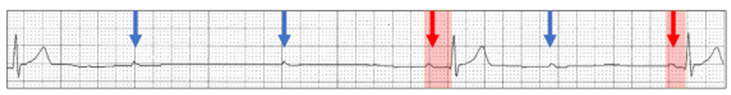
Abrupt sinus bradycardia (red arrows):
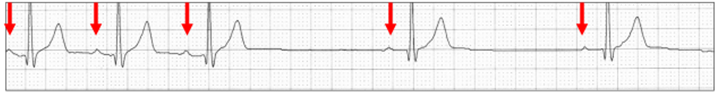
Abrupt termination of sinus bradycardia (red arrows):
An abrupt sinus slowing (red arrows) may allow an ectopic atrial focus (green arrows) to emerge:

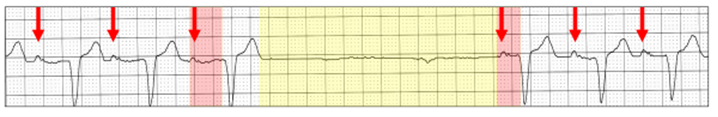
When the sinus pacemaker slows sufficiently, the AV node may emerge as the intrinsic cardiac pacemaker. The result can be competitive pacemaker rhythms between the two nodes referred to as iso-rhythmic AV dissociation.
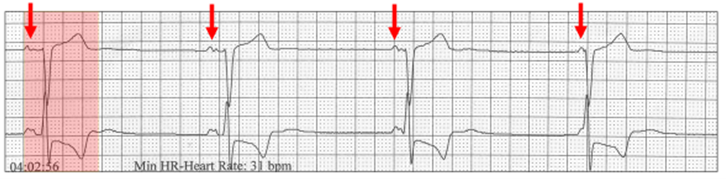
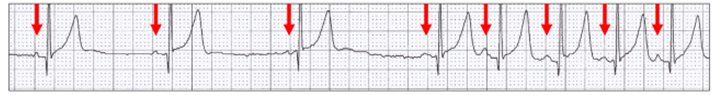
The sinus rate is 30 bpm (red arrows). The first complex has normal AV conduction (red highlight). The PR intervals then shorten as the QRS complexes from a junctional pacemaker are slightly faster than the sinus P wave rate. These changes in AV delay are “rhythmic” because of respiratory sinus arrhythmia.
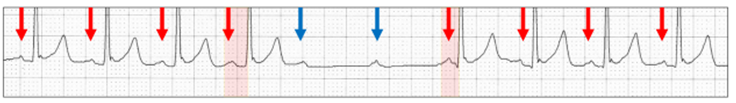
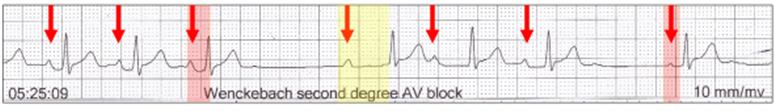
With vagal hypertonia the AV node is frequently involved. Wenckebach AV sequences are extremely common, and most can be regarded as physiologic.
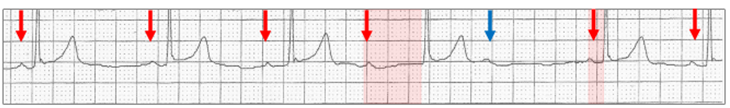
Wenckebach AV sequence (red highlight), The dramatic, abrupt change in the AV delay occurs immediately before the dropped beat (blue arrow), with no change in the sinus rate (red arrows) confirming transient vagal hypertonia.
The same abrupt change in the AV delay (red highlight) can occur with an ectopic atrial rhythm (green arrows).
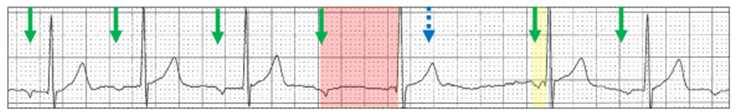
The dropped P wave (blue stippled arrow) is concealed. The first AV delay after the dropped beat is very short (yellow highlight) suggesting the QRS is a junctional escape beat. Maybe, the QRS with the long AV delay is also a junctional escape beat and there are two dropped P waves.
This is real fun!
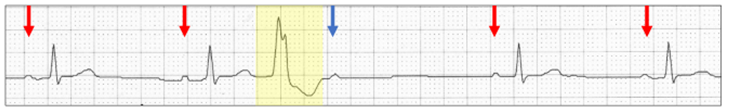
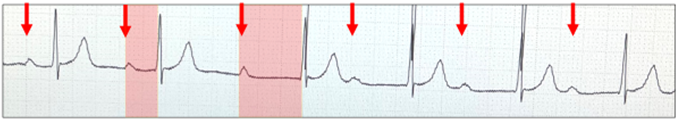
Wenckebach AV sequence (red highlight) with two dropped P waves (blue arrows) and no real sinus slowing (red arrows).
Now let us visualize an amalgam of parasympathetic activity from both vagal nerves.
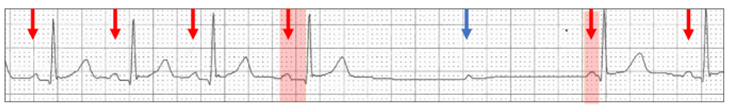
There is sinus rhythm (red arrows) with abrupt sinus slowing together with a Wenckebach AV block sequence (red highlight) and a dropped P wave (blue arrow).
In this scenario, there are frequent junctional escape beats (yellow highlight).
One has to ask if this is really physiologic?
Sinus rhythm (red arrows) with a Wenckebach AV sequence (red highlight) and no dropped P wave but rather sinus arrest (yellow highlight):
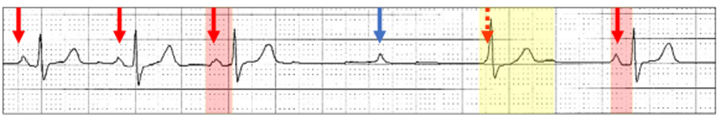
Ventricular ectopics during vagal hypertonia can cause diagnostic confusion.
Sinus bradycardia (red arrows) with a premature ventricular ectopic (yellow highlight) followed by a dropped P wave (blue arrow). There is no change in the PR intervals. Is this a Wenckebach AV block sequence interrupted by a ventricular ectopic? The PR intervals are fixed. The non-conducted P wave would normally be concealed within the ectopic, but because of sinus bradycardia it now lies beyond the T wave, but AV conduction is still refractory.
With ventricular ectopics, partial refractoriness can lead to bizarre ECG appearances and in particular, what I call pseudo-reversed Wenckebach.
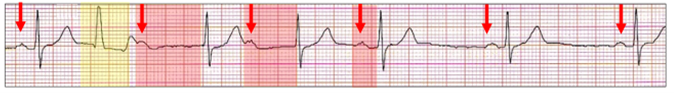
The rhythm is slow sinus (red arrows) and there are no dropped P waves. A premature ventricular ectopic (yellow highlight) results in the next P wave lying beyond the ectopic T wave. However, AV conduction is now possible but with a very significant AV delay (red highlight). This results in the next P wave also lying just beyond the T wave and also partially refractory. The PR interval then returns to normal. This is similar to a reversed Wenckebach AV block which also does not have a dropped P wave although in this case it is physiologic and dependent on timing. Note that despite the pause the ventricular ectopic is interpolated!
This ECG would be impossible to understand unless we understand the eccentricities of vagal hypertonia.
There is a regular sinus rhythm (red arrows). The AV delay (red highlight) lengthens significantly as a result of abrupt vagal hypertonia at the AV node, which persists through the tracing.
In this similar ECG, both the sinus and AV nodes are involved.
There is episodic sinus slowing (red arrows). The AV delay initially lengthens (yellow highlight) and then returns to a normal AV delay (red highlight) with the appearance of a reversed Wenckebach sequence and no dropped beat.
One can only imagine the complex interplay of the sympathetic and parasympathetic nervous systems at both the sinus and AV nodes in the young and in particular the elite athlete.
In 49+ years as a practicing cardiologist, Dr Harry Mond has published 260+ published manuscripts & books. A co-founder of CardioScan, he remains Medical Director and oversees 500K+ heart studies each year.
Download his full profile here.